Can You Become Paralyzed From Degenerative Disc Disease – Find Out How To Protect Yourself!
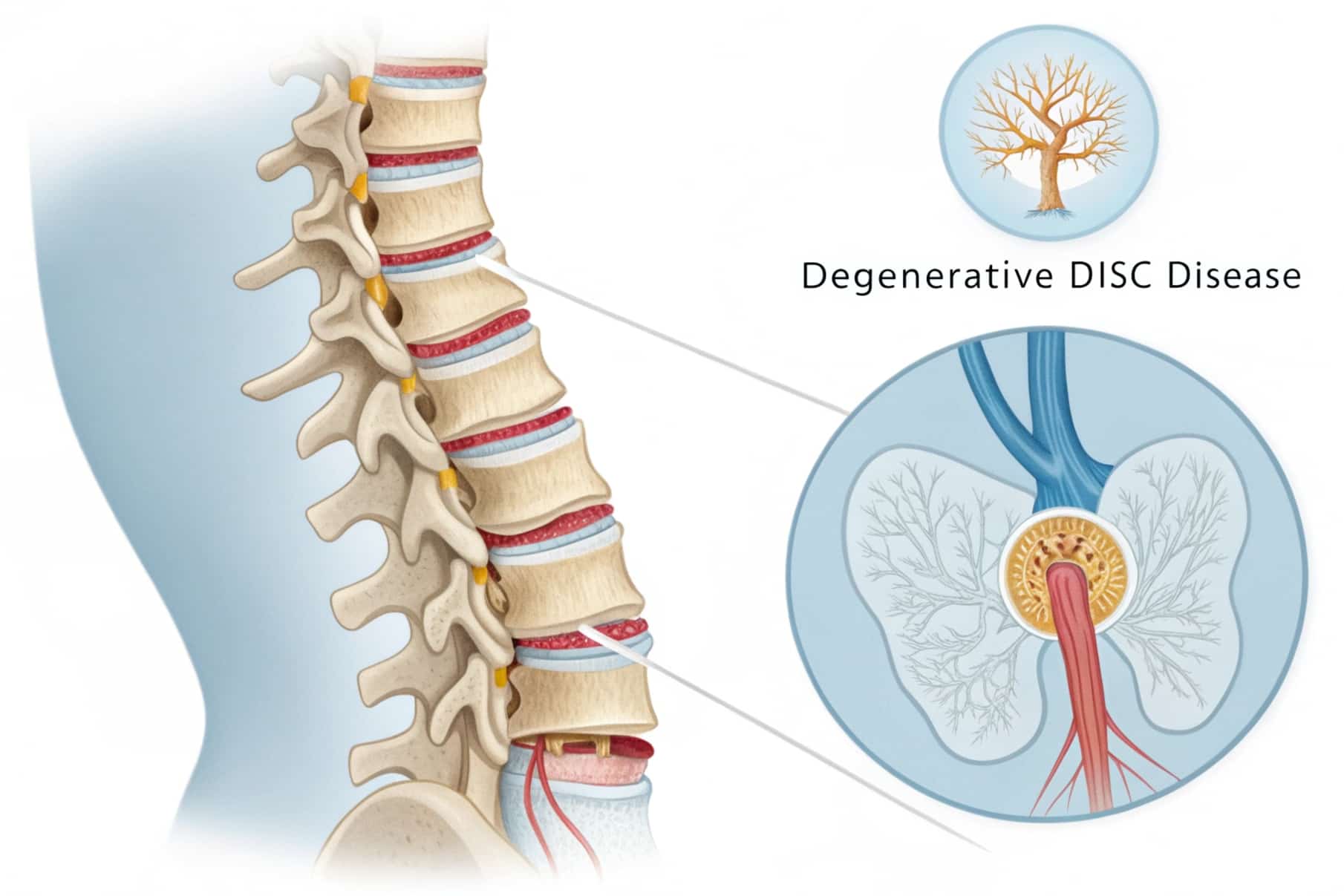
Degenerative Disc Disease, also known as DDD, is a condition that affects millions of people around the world. It happens when the discs between the bones in the spine begin to wear down over time. These discs are soft cushions that help the spine move smoothly. As they break down, they can cause pain, weakness, and other problems in the back or neck.
Some people worry that DDD can cause serious issues like paralysis. While this fear is understandable, the truth is that paralysis from degenerative disc disease is extremely rare. It usually only happens when the condition becomes very severe and is left untreated for a long time. Most people with DDD will never face such a serious outcome.
This article explains everything you need to know about degenerative disc disease in simple language. It also gives a clear look at the symptoms, causes, treatment options, and when there may be a small risk of paralysis. A helpful table is included to break the information down even more clearly.
What is Degenerative Disc Disease?
Degenerative Disc Disease is a condition where the discs between the bones in the spine wear down due to aging, injury, or stress. These discs act like cushions and help the spine move smoothly. When they begin to break down, they lose flexibility and can cause pain, stiffness, and reduced motion.
Common symptoms include back or neck pain, tingling or numbness in the limbs, and muscle weakness. It mostly affects the lower back (lumbar spine) and the neck (cervical spine). Although it sounds serious, it usually develops slowly and can be managed with proper care.
What Is Degenerative Disc Disease and Can It Lead to Paralysis?
| Topic | Details |
| What is it | A condition where spinal discs wear out over time |
| Common areas affected | Neck (cervical spine), lower back (lumbar spine) |
| Main symptoms | Pain, numbness, stiffness, weakness |
| Risk of paralysis | Very rare, but possible in severe, untreated cases |
| Related conditions | Spinal stenosis, herniated disc, cauda equina syndrome |
| Causes | Aging, poor posture, injury, genetics, and smoking |
| Treatments | Medication, physical therapy, and surgery in serious cases |
How Degenerative Disc Disease Affects the Spine?
As people age, their spinal discs naturally lose water and elasticity. This process makes them thinner and less flexible. Over time, the disc may begin to crack or bulge. When this happens, it can press on nearby nerves or even the spinal cord in more serious cases.
This pressure on the nerves may cause symptoms such as:
- Burning or sharp pain
- Tingling in the hands, arms, legs, or feet
- Muscle spasms
- Difficulty walking or standing for long periods
In rare situations, if the nerves or spinal cord are severely compressed, it may affect the body’s ability to control movements or feel sensations. This is when the risk of paralysis becomes a concern, although it is not common.
When Does Degenerative Disc Disease Lead to Paralysis?
Paralysis happens when the communication between the brain and the body is cut off. This can occur if the spinal cord is seriously damaged or pinched for an extended period. In the case of DDD, paralysis is not typical but may happen due to the following reasons:
Severe Nerve Compression:
Paralysis can occur if a degenerated disc presses heavily on spinal nerves or the spinal cord for a long time. This pressure can damage the nerves permanently, disrupting signals between the brain and body, which may cause weakness or loss of movement in affected areas.
Spinal Stenosis:
Spinal stenosis happens when the space around the spinal cord narrows, often due to degenerative disc disease. If severe, this narrowing can compress nerves and block nerve signals, potentially causing numbness, weakness, or paralysis if left untreated over time.
Herniated or Bulging Discs:
When a disc’s outer layer breaks, the inner material may bulge out and press on nearby nerves or the spinal cord. This can cause pain and, in rare, severe cases, disrupt nerve communicatio,n leading to paralysis if the pressure is intense and persistent.
Cauda Equina Syndrome:
Cauda Equina Syndrome affects the lower spinal nerves and is a medical emergency. It causes sudden leg weakness and loss of bladder or bowel control. Without urgent treatment, this syndrome can lead to permanent paralysis in the lower body and requires immediate medical care.
Also read: Is Gum Disease Hereditary – Simple Ways To Lower Your Risk Starting Now!
Symptoms That Need Immediate Attention – These Signs Could Be Dangerous!

Most people with DDD experience only mild to moderate symptoms. However, certain signs should never be ignored. These may signal a more serious issu,e such as nerve damage:
- Sudden Numbness or Tingling
If you suddenly lose feeling or notice numbness in your arms or legs, it could mean nerves are being compressed or damaged. This loss of sensation can affect your balance and coordination. - Difficulty Walking or Weakness
Feeling weak in your legs or having trouble walking steadily may indicate that the nerves controlling your muscles are affected. This can increase the risk of falls or injury. - Problems with Hand Grip or Fine Motor Skills
Difficulty holding objects or releasing your grip can signal nerve irritation in the neck or upper spine. This can affect daily tasks like writing, buttoning clothes, or using utensils. - Loss of Bladder or Bowel Control
Losing control over urination or bowel movements is a serious sign. It suggests that nerves controlling these functions are compressed, requiring urgent medical attention to prevent permanent damage. - Persistent and Severe Pain
Intense shooting or burning pain that doesn’t improve with rest or medication may be a warning that the nerve damage is worsening and needs immediate evaluation and treatment.
If you experience any of these symptoms, do not wait. Contact a healthcare professional immediately to avoid serious complications, including paralysis. Early intervention can help protect your nerve function and quality of life.
Causes and Risk Factors of Degenerative Disc Disease – Don’t Ignore These Triggers!
Aging:
As we age, our spinal discs lose water content and become less flexible. This natural process weakens their ability to absorb shock. Most people over 30 experience some disc wear, but when it becomes painful or limits movement, it may be diagnosed as degenerative disc disease, especially in the lower back or neck area.
Genetics:
Genetic makeup plays a strong role in disc health. If your parents or close family members have a history of DDD, you might inherit weaker discs. Even with a healthy lifestyle, some people naturally have discs that wear down more quickly, making them more likely to experience early symptoms of degenerative disc disease.
Smoking:
Smoking decreases oxygen and nutrients delivered to the spinal discs by reducing blood flow. This leads to faster disc breakdown, inflammation, and poor healing. Smokers are also more prone to chronic pain, meaning smoking not only raises the risk of DDD but also worsens the symptoms and slows recovery if disc damage occurs.
Poor Posture:
Maintaining poor posture over time places uneven pressure on spinal discs. Whether sitting hunched over or standing with bad alignment, this strain accelerates disc wear. The constant imbalance weakens the spine’s support system and raises the risk of developing DDD, especially in people who sit for long hours or lift incorrectly.
Repetitive Strain:
Jobs or hobbies involving frequent lifting, bending, or twisting place repeated stress on the spine. Over the years, this movement damages discs slowly. Factory workers, athletes, and laborers are especially at risk. Without proper support or posture, these actions can cause small disc injuries that build up and lead to long-term degeneration.
Obesity:
Excess body weight increases pressure on spinal discs, especially in the lower back. This constant load speeds up disc deterioration, reducing flexibility and increasing pain. Obesity is linked with faster DDD progression, and the extra weight may also worsen inflammation in surrounding joints and tissues, leading to additional back problems and discomfort.
How Is Degenerative Disc Disease Diagnosed by Doctors?
Doctors diagnose Degenerative Disc Disease through a mix of physical exams and imaging tests. First, they check your spine’s flexibility, look for areas of tenderness, and see if pain travels to your arms or legs. They may also assess nerve function.
To get a clearer view, doctors often use X-rays to examine disc space and bone changes, MRIs to view disc damage and soft tissues, and CT scans for detailed images of bones and nerves. These steps help confirm the diagnosis and check if nerves are affected or compressed.
Treatment Options for Degenerative Disc Disease – Expert Tips for Faster Recovery!
Treatment depends on how serious the symptoms are. Most people find relief with non-surgical treatments.
Medications:
Doctors usually start treatment with medicines to manage pain and inflammation. Over-the-counter drugs like ibuprofen or acetaminophen help reduce general discomfort. If muscle spasms occur, muscle relaxants may be prescribed. In cases involving nerve pain, doctors may give prescription medications such as gabapentin or pregabalin, which are designed to calm irritated nerves.
Physical Therapy:
Physical therapy is often one of the most effective non-surgical treatments. A trained therapist will guide you through stretches and exercises that improve flexibility, posture, and core strength. This not only reduces pain but also supports the spine, helping to prevent further disc damage. Over time, physical therapy may improve daily function and reduce reliance on medication.
Lifestyle Changes:
Small changes in everyday habits can have a big impact:
- Losing excess weight helps reduce pressure on the spine.
- Practicing proper posture while sitting, standing, or lifting can prevent extra strain.
- Low-impact activities like walking, swimming, or yoga keep the body flexible and the muscles strong, which helps manage symptoms better.
Injections:
If pain is severe and doesn’t improve with therapy or medicine, corticosteroid injections may be used. These are injected near the affected disc to reduce inflammation and provide temporary pain relief, especially if nerve roots are inflamed. However, they are not a long-term solution and are used sparingly.
Surgery (For Severe Cases):
Surgery is only recommended when all other treatments fail and the pain becomes disabling or nerve damage begins to occur. Here are the common options:
- Discectomy: The surgeon removes the damaged part of the disc that’s pressing on a nerve.
- Spinal Fusion: Two or more vertebrae are permanently joined to stabilize the spine and stop painful movement.
- Artificial Disc Replacement: The damaged disc is replaced with a man-made one that maintains normal spine motion.
While surgery carries risks, it often brings significant relief if performed under proper conditions by an experienced surgeon.
Also read: Coach Yplostylia Varkonin Health – Real Results, Real Wellness!
How to Prevent Degenerative Disc Disease from Getting Worse?

While you can’t always stop disc degeneration, you can reduce the chance of serious complications:
- Exercise Regularly: Gentle exercises like walking, swimming, or yoga can keep your spine flexible and strengthen back muscles. Stronger muscles offer better support for the spine and reduce pressure on the discs, which helps slow down further damage caused by degenerative disc disease.
- Maintain a Healthy Weight: Excess weight, especially around the abdomen, increases the stress on spinal discs. By maintaining a balanced diet and engaging in regular physical activity, you can reduce the burden on your spine and help prevent the worsening of disc degeneration over time.
- Quit Smoking: Smoking limits oxygen and nutrient supply to spinal discs, causing them to wear out faster. Quitting smoking not only improves blood circulation but also allows the spine to heal better and lowers the risk of advanced degeneration and related complications.
- Use Good Posture and Ergonomics: Sitting, standing, or lifting with poor posture strains the spine. Using ergonomic chairs, proper back support, and adjusting your workstation can reduce pressure on discs, improve alignment, and lower your chances of worsening degenerative disc disease symptoms.
- Avoid Heavy Lifting and Repetitive Strain: Lifting heavy objects incorrectly or doing repeated spine-stressing movements can speed up disc wear. Use safe lifting techniques, avoid bending or twisting too often, and take regular breaks if your job or routine involves repetitive back motion.
FAQS:
1. How bad is degenerative disc disease?
Degenerative disc disease varies in severity. For many, it causes mild to moderate back or neck pain and occasional stiffness. However, for some, it can lead to chronic pain and reduced mobility. Early diagnosis and proper management, like exercise and medication, can help control symptoms and improve quality of life.
2. Does degenerative disc disease affect life expectancy?
Degenerative disc disease does not affect life expectancy. It mainly causes pain and discomfort but is not life-threatening. Most people live normal, healthy lives with proper treatment, including physical therapy and lifestyle changes. Managing symptoms well helps maintain daily activities without reducing lifespan.
3. How to stop degenerative disc disease from progressing?
To slow down degenerative disc disease, keep your back muscles strong through regular exercise, maintain a healthy weight, and avoid smoking. Practice good posture and ergonomics, lift objects carefully, and take breaks if sitting long. These habits reduce stress on your spine and help protect your discs from further damage.
4. Can you go paralyzed from degenerative disc disease?
Paralysis from degenerative disc disease is rare but possible. It may occur if a severely damaged disc compresses the spinal cord or nerves for too long. Conditions like spinal stenosis or cauda equina syndrome linked to advanced DDD can cause nerve damage, which requires urgent medical treatment to prevent paralysis.
5. When should I see a doctor for degenerative disc disease?
You should see a doctor immediately if you experience sudden numbness or weakness in your arms or legs, severe pain that does not improve, or loss of bladder or bowel control. These signs suggest serious nerve damage, which requires prompt medical evaluation and treatment to avoid permanent problems.
Conclusion:
Degenerative Disc Disease is a common condition that causes back and neck problems for many people. While it can be painful and affect daily life, the risk of becoming paralyzed from this condition is extremely low. In most cases, people manage DDD successfully with non-surgical treatments like physical therapy, medication, and healthy lifestyle changes.
However, ignoring serious symptoms or avoiding medical advice may lead to complications, including nerve damage. That’s why early diagnosis, proper care, and regular monitoring are very important. If treated in time, degenerative disc disease rarely leads to paralysis, and most people continue to live active, independent .
Related post: